Supporting people
1
People can find and register with Future Pathways
Of the 1,289 people who have ever registered with us, 1,051 (82%) have received support. The heart of this is a conversation – or more often several – with a Support Coordinator, in which the person works out what kind of support will be most helpful for them.
“The way they deal with you is very important. It is a breath of fresh air after the way you are treated by police….They don’t have lots of forms, you will mention something to [Support Coordinator] and they will either say Yes or No – no bargaining, and that is really important to people who have been in care. The whole team is really nice. I value getting trusted advice from people who understand the process and issues.”

2
People value our trauma-informed approach, which embodies the principles of Choice, Empowerment, Safety, Trust and Collaboration.
Many people talk about the importance of trust. When we ask people how they felt during their first conversation with their Support Coordinator, they often say “relieved” and “believed”.
We know that we cannot help people until we have built up rapport and mutual trust. That takes time.
We do not ask for evidence from people’s experience in care. This is very important to them, and helps to build trust, even though many of them find it difficult to trust institutions and professionals.
Collaboration is also vital. People tell us that they feel safe and listened to, and that their opinions are valued. A key part of this is Future Pathways being flexible: we give people choices about where, when and how they talk to us.
NHS Education Scotland defines trauma-informed practice as follows:
Trauma-informed practice is not designed specifically to treat trauma-related difficulties. Instead it seeks to address the barriers that those affected by trauma can experience when accessing the care, support and treatment they require for a healthy life. It is argued that those most in need may also be hardest to reach and most unlikely to engage with services. Trauma-informed practice seeks to ensure that services:
- • recognise that trauma is common
- • realise that a person’s trauma may impact the way a service is delivered, for example, using a person centered approach respond safely and effectively, ensuring that those who require support are referred for and receive the necessary trauma specific interventions for recovery
- •Resist re-traumatisation by ensuring that services are delivered safely and in line with the key principles of:
- – choice
- – collaboration
- – trust
- – empowerment
- – safety

3
People know what is important to them and what resources they need
A lot happens before we agree resources and put plans into action. We talk to people; we focus on what changes they want to make in their lives; we plan the support they need; and we try to make sure that the person clearly sees benefits of Future Pathways’ approach.
In terms of the specific details of the support, this can vary widely as, of course, each person is different. But we do see some broad themes around what is important to people:


Having a routine, hobbies and volunteering

Social networks and community activity

Hope for the future

Increased physical activity and improved wellbeing

Self-care and Self-reflection; valuing myself

Financial stability

4
Future Pathways helps people to live the life they want
We will illustrate this point by telling Debbie’s story.
Debbie is a focused and determined young woman who lives on the west coast of Scotland. When she registered, she hoped to get help to find her records.
Debbie and her Support Coordinator had several conversations. Debbie described frequent panic attacks when meeting new people. This could cause problems when she was trying to use services: for example, she had been de-registered from a GP surgery list after speaking to staff aggressively.
Debbie wanted to find better ways of coping with stressful, painful, or frustrating situations. Future Pathways arranged for mindfulness coaching sessions.
On the way to her first session, Debbie had a panic attack and could not attend. She was surprised that the mindfulness coach later called to check on her. The coach’s understanding and sensitive approach helped her to decide to try again.
At first, Debbie relied on taxis to get to the sessions (Future Pathways organised these). Now, though, the coach has helped establish a safe and comfortable environment for her, and she could make her own travel arrangements.
Debbie has learned positive coping strategies to ‘calm down and be healthy’ when negative situations occur. The mindfulness sessions have also helped Debbie to think about how her stress and distress affects her, and how this may in turn affect her communication with others.
She now feels more confident in how she communicates with other people, and notices a positive difference in how she engages with people and services more generally. We asked her what it is now like for her to go to her GP, and she said: “I see the difference in how [the staff] respond to me now.”

5
Change is happening, but barriers still exist
Future Pathways is clearly doing a lot of good. As problems have arisen we have dealt with them.
At the time of writing, we have supported 1,059 people – that’s 82% of those who registered with us. We know that this has made a big difference to people’s lives.
And we work well with our partners. Access to material support has been greater than expected and hugely valued, enhancing quality of life in ways that no service might achieve. More than £3.6 million was accessed by 73% of the people that received support so far. We have used this money in a large variety of ways, depending on the particular needs of each person.
1. 2016/17 includes data for only six months
2. 2019/20 includes data for only nine months
3. Average amount per person in 2019/20 is equivalent to £3,176 in a full year.
Here’s how the Discretionary Fund has been used

Home Safety & Comfort
£984, 826

Vehicle
£590, 612

Travel / Accommodation
£352, 548

Miscellaneous
£250, 457
Furniture
£222, 969

Trip
£177, 607
Access to Courses / Education
£125, 325
Health & Fitness
£109, 709

Funeral
£108, 173

Travel
£107, 803

Computer
£99, 600

Clothing & Personal Care
£78, 333

Business Support
£67, 851

Hardship
£57, 766

Complementary Therapies
£44, 796

Dental
£43, 896

Driving Lessons
£40, 483

Unknown
£28, 361

Short Term Purchased Support
£13, 947

Record Search / Genealogy
£4, 280
Total: £3,509,340
1. This information is based on over 7500 financial records. Data was cleaned and then cross checked with paper files, however not all data was recorded in sufficient detail for coding, particularly during the initial start up period. For these reasons it has not been included here.

There are some barriers that we will have to overcome in future, however. We see two in particular:
1. Support Coordinators having to take responsibility for things that other services could do
Many survivors do not trust statutory services or professionals, and would prefer to access support directly from Future Pathways. However, this can be a problem in situations where, in fact, other services are better placed to respond.
2. People having difficulty accessing public services
These might be social work, occupational therapy, housing, benefits, or other services. People struggle to access them for a variety of reasons.

A Support Coordinator shares their experience of helping someone who required input from numerous services and supports.
I supported someone who attended frequent appointments with multiple health services. They had several physical and mental health diagnoses and there did not appear to be a plan to coordinate the services’ input. The appointments were difficult for the person to manage. Having to repeat their current situation and their history was extremely distressing.
It could take several months for a referral to result in an appointment. Quite often, appointments would be changed or cancelled. The impact of this was that the person was not always able to attend appointments. Sometimes they presented what was seen as difficult or disruptive behaviour in service locations like GP practices. The person would then be prematurely discharged from services. Being without a GP for any length of time would be extremely detrimental to this person, and result in issues with medication and potentially benefit entitlements.
For people who have experienced trauma, new environments, meeting new people and changes to routine can cause huge levels of anxiety. It is also common for people that we support to have a mistrust of services, particularly statutory services, due to their past experiences. For example, waiting in a social work office can bring back negative memories and associations which can result in that person re-experiencing and re-living traumatic events. It can take careful planning and supportive conversations before someone agrees to meet with professionals.
I felt it was important for this person to have some regular, practical support and assistance around managing these appointments. I requested a meeting with of the involved services; the person’s GP, a specialist dietician, the social work addictions service, representatives from the mental health team, a private counsellor, and support staff from two of Future Pathways delivery partners who had worked with the person.
This meeting was organised by the addictions service. None of the other involved services attended, however some offered input for me to communicate at the meeting. The social worker attached to the addictions service shared that they planned to discharge the person. There were no alternative supports in place; although it was recognised there were many areas where support was needed because the person’s health and wellbeing was at risk. The social worker agreed that a community care assessment would be important.
After the assessment, a meeting was held with several professionals to discuss what statutory support was available and appropriate. The person was not invited to this meeting, but we agreed I would advocate on their behalf. After this, we discussed the proposed supports with the person who was able to share how they felt about what was suggested. They had input and control over how the care plan was developed.
There is now a coordinated support plan in place with weekly input through the community social work team. An expanded support network is building; the person now has a trusting relationship with a worker from a statutory service so it has been easier to establish connections with other supports. The person is visiting the GP and hospital less frequently and has built a better relationship with their GP because their needs are better understood. Regular reviews with the community social work team also ensures the person’s views are heard.

6
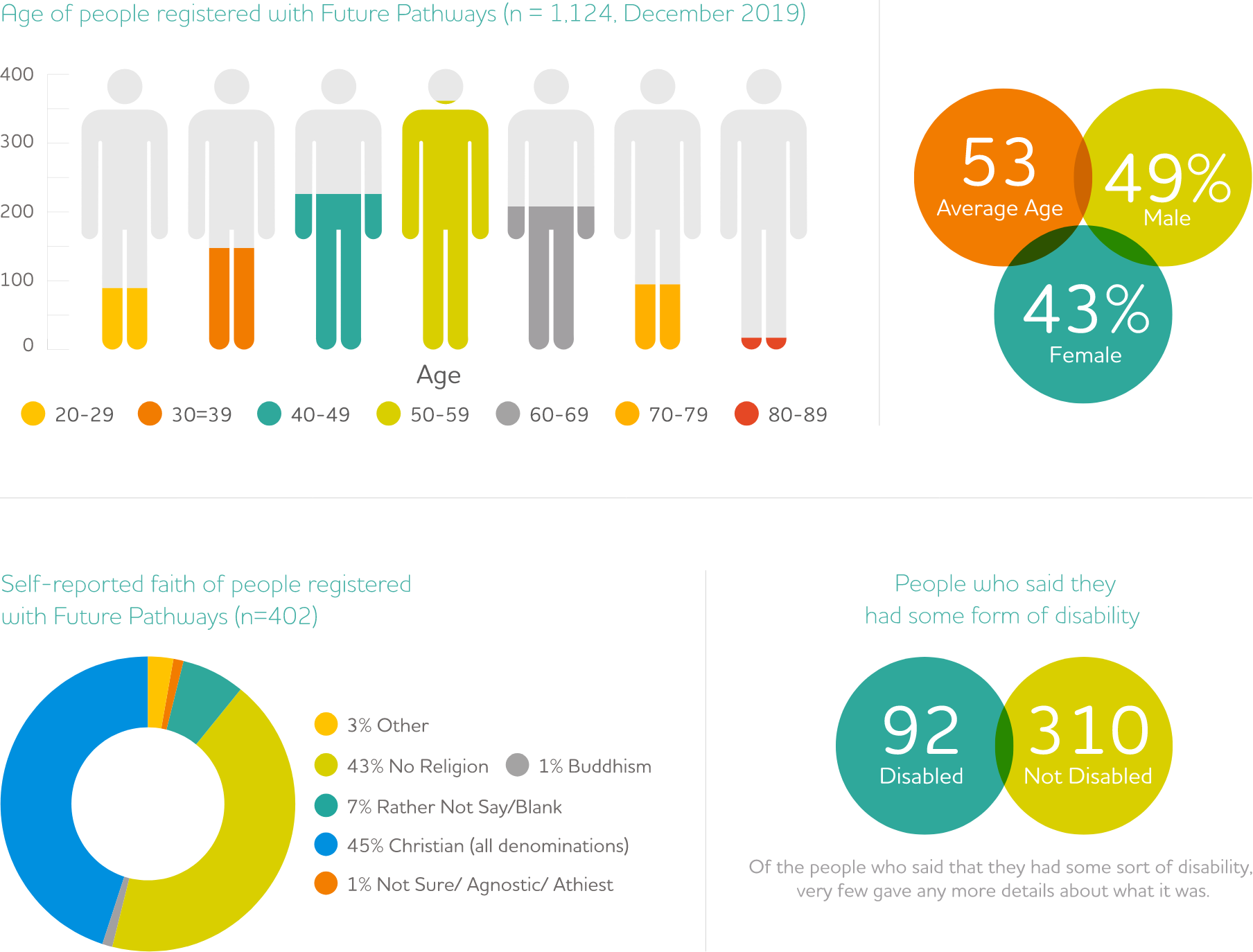
Future Pathways works with a varied mix of people
We ask people who register with us about their ethnicity, faith and so on. People do not have to answer any questions that they do not want to, so we do not have to complete information on this. Based on what we do know, it breaks down like this.
7
People who register with us are more likely to live in deprived areas
We analysed the postcodes of 1,141 people registered with us who lived in Scotland. We found that they are more likely to live in deprived areas (according to the Scottish Index of Multiple Deprivation).
The Scottish Index of Multiple Deprivation
The SMID divides Scotland into 6,976 small areas, called data zones, and measures seven things: income, employment, education, health, access to services, crime, and housing. It is used by the Scottish Government, and many other organisations.
